Temporary pacing
Temporary pacing
Temporary pacing is a life saving procedure for maintaining the heart rate when it falls markedly producing features of cerebral hypoperfusion. It can also be done prophylactically during certain procedures when there is a possibility of sudden fall in heart rate. Other reasons for temporary pacing are pacing to overdrive a tachycardia like ventricular tachycardia and pacing at fast rate to stabilize an aortic balloon valvuloplasty balloon during balloon valvuloplasty. Temporary pacing is done prior to permanent pacing, to give a good bradycardia support during the procedure. For the same reason, it is used prior to complex interventional procedures, though you may occasionally end up with a temporary lead perforation after a successful interventional procedure!
Temporary transvenous pacing
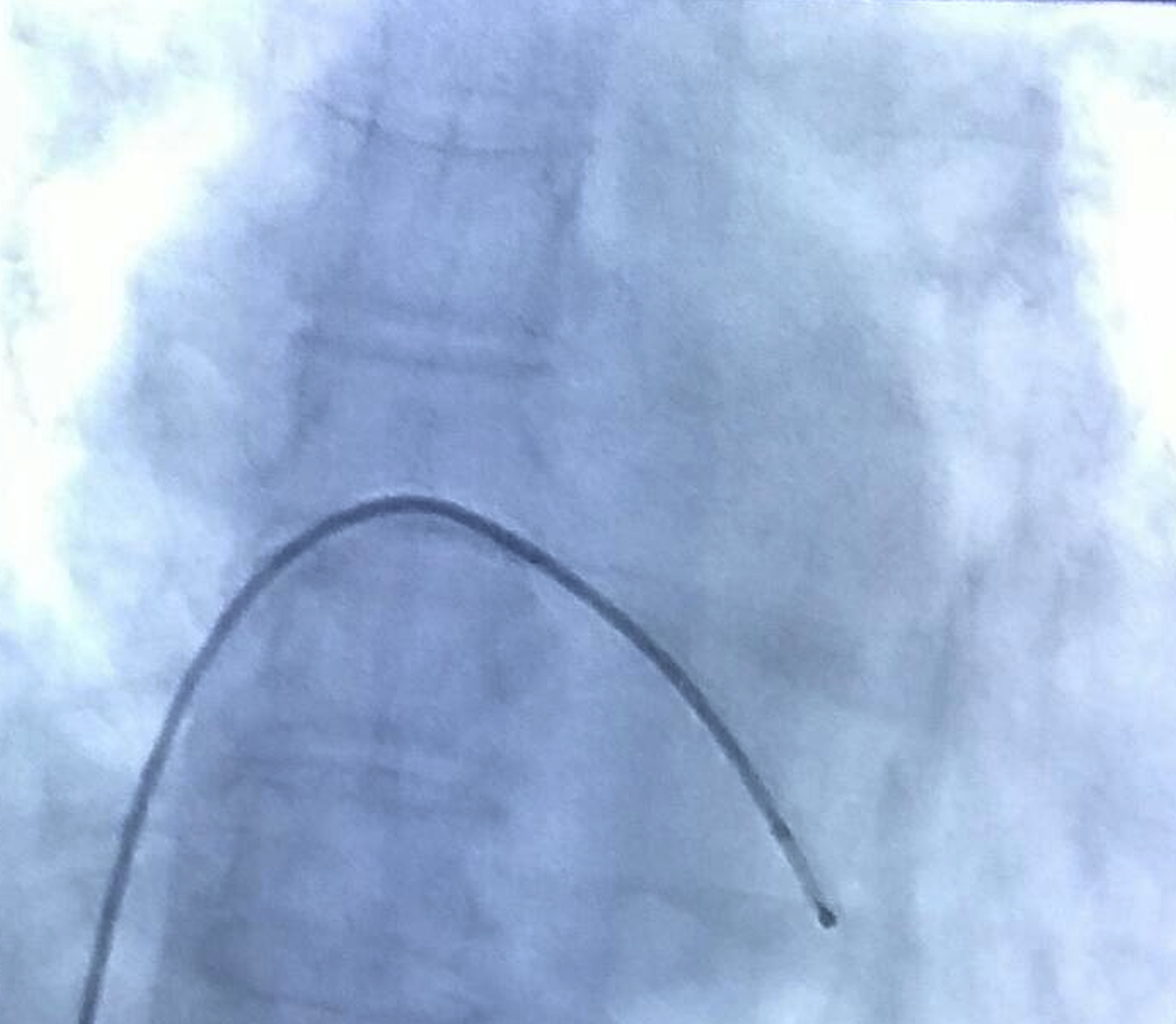
The fluoro shot shown above is that of temporary transvenous pacing through the femoral vein. The pacing lead is introduced through percutaneous puncture of the femoral vein in the groin. Lead is introduced under fluoroscopic control through the inferior vena cava and right atrium into the right ventricular apex. Pacing threshold is checked using the pacing system analyzer or a temporary pacemaker and the output kept 2-3 times above the threshold, to ensure regular pacing. Externally the pacing lead is fixed to the skin to reduce the chance of migration. Temporary transvenous pacing can also be done from the jugular (transjugular pacing) or subclavian routes by percutaneous puncture. Pacing maneuvers are an integral part of an electrophysiology study. In this case pacing is done from various locations unlike the usual right ventricular pacing for bradycardia support.
Transvenous pacing can also be done at the bedside using balloon tipped flow directed catheters introduced by a subclavian puncture. Electrocardiographic monitoring from the tip of the pacing lead can guide us on the chamber in which the lead tip is positioned, in the absence of fluoroscopy at the bedside. While the tip is in the right atrium, large atrial deflections are recorded, and the pattern changes to an intracardiac ventricular electrogram when the lead tip reaches the right ventricle.
Pacing through the coronary artery
Pacing through the coronary artery is done as an emergency measure when a patient develops severe bradycardia during a coronary intervention procedure, if a temporary transvenous catheter is not already in place. The proximal end of the coronary guide wire can be connected to the temporary pacemaker using a crocodile clip. A needle stuck into the skin can serve as the second electrode. This saves time needed for achieving an urgent femoral venous puncture and sometimes the potential bleeding risk of such punctures in a person who is fully anticoagulated for the coronary intervention.
Non invasive transcutaneous temporary pacing
Pacing in an emergency situation can be obtained in the intensive care unit using external pacers which pace through large adhesive electrode patches applied to the chest wall. The disadvantages of transcutaneous pacing are the large current needed and consequent pain due to skeletal muscle stimulation as well as the often unreliable ventricular capture. At the most it can be used in standby mode to buy time for arranging a transvenous pacing.
